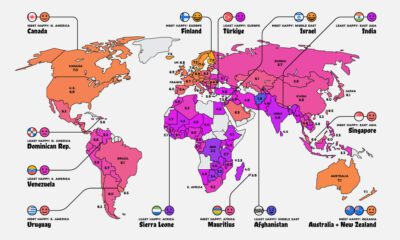
While most of us are experiencing higher levels of emotional distress than normal, the severity of stress may change based on factors such as age, race, education level, or even where you live. This graphic uses data from the National Pandemic Emotional Impact Report to illustrate how each demographic subgroup in the U.S. is feeling.
The Methodology
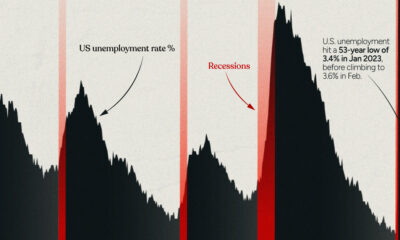
The emotional upheaval of such a unique event impacts people in different ways, and is difficult to measure given the many direct and indirect factors associated with it. For the report referenced in the graphic, researchers created a detailed methodology to measure the impact of COVID-19 across a sample of 1,500 adults. Surveys were conducted in May 2020, when the majority of people were under strict lockdown orders. Unemployment levels mirrored those seen only during the Great Depression, and of course, the death rate was rising quicker than anyone could have anticipated. A Pandemic Distress Index Score (PDIS) was calculated based on participant’s responses, which were then divided into low (bottom 25%), moderate, and high (top 25%) quartiles of pandemic distress.
Emotional Distress Levels, by Demographic Group
Findings uncovered that almost 40% of participants have lost their jobs, or experienced a reduction in income due to the COVID-19 outbreak. However, the reverberations of such stressors vary by demographic subgroup.
Age
According to the report, pandemic-related emotional distress decreases by age group. People in the 18-34 year bracket reported the most pandemic-related distress overall—with respondents citing high stress at nearly double the rate of people over 50 years old. Meanwhile, respondents in the 65+ age group had reported the lowest distress scores of all.
Race
Of all ethnicities in the survey, Hispanics/Latinos and Blacks had the highest average Pandemic Distress Index Scores, and Whites had the lowest average scores. It is also worth noting that the research concluded five days after the death of George Floyd, so the majority of responses may not include the influence of this event, and the subsequent movement against systematic racism.
Other Categories
In other subgroups, there were slight differences worth mentioning. For example, from a communities perspective, people who live in rural areas were less likely to experience high pandemic distress compared to people living in towns or cities. When it comes to the battle of the sexes, men and women experience similar levels of distress. Moreover, the level of emotional distress related to COVID-19 did not differ much between people with children under 18 and those with older children. However, women with children under 18 reported more symptoms of anxiety compared to women with no minor children.
What Does the Data Mean?
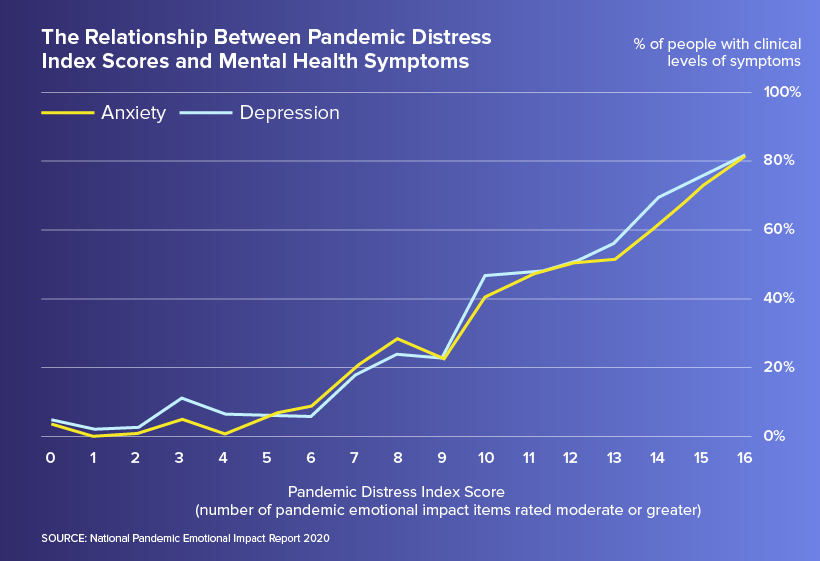
While the research presents several important insights, understanding what it means is crucial in providing people with the support they need. For example, participants with high pandemic-related distress are 40 times more likely to have clinically significant levels of anxiety and 20 times more likely to have clinically significant symptoms of depression, compared to those on the lower end of the spectrum.
In fact, a report from the Center for Disease Control and Prevention shows that 1 in 4 people in the 18-24 age bracket have seriously considered committing suicide at some point during the month of June 2020, which is in line with the emotional distress scores for this age group.
Building Immunity
While nobody can escape the devastating impacts of COVID-19 on mental health, it is clear that some people are more at risk than others. Unfortunately, younger adults and people of racial and ethnic minorities have carried higher psychological burdens from the pandemic so far, and we have yet to see the long-term effects that could transpire as a result. —António Guterres, United Nations Although at times the pandemic may feel inescapable, we must continue to prioritize both our physical and mental health—so we can build immunity for what’s to come. on In the above infographic from NuGen Medical Devices, we explore the factors leading to the syringe shortage and take a look at the company’s innovative needle-free solution that could play an important role in closing the immunization gap.
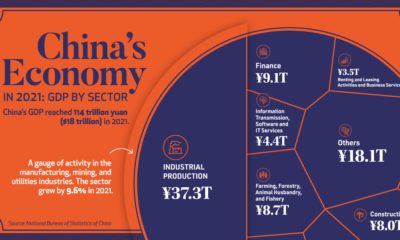
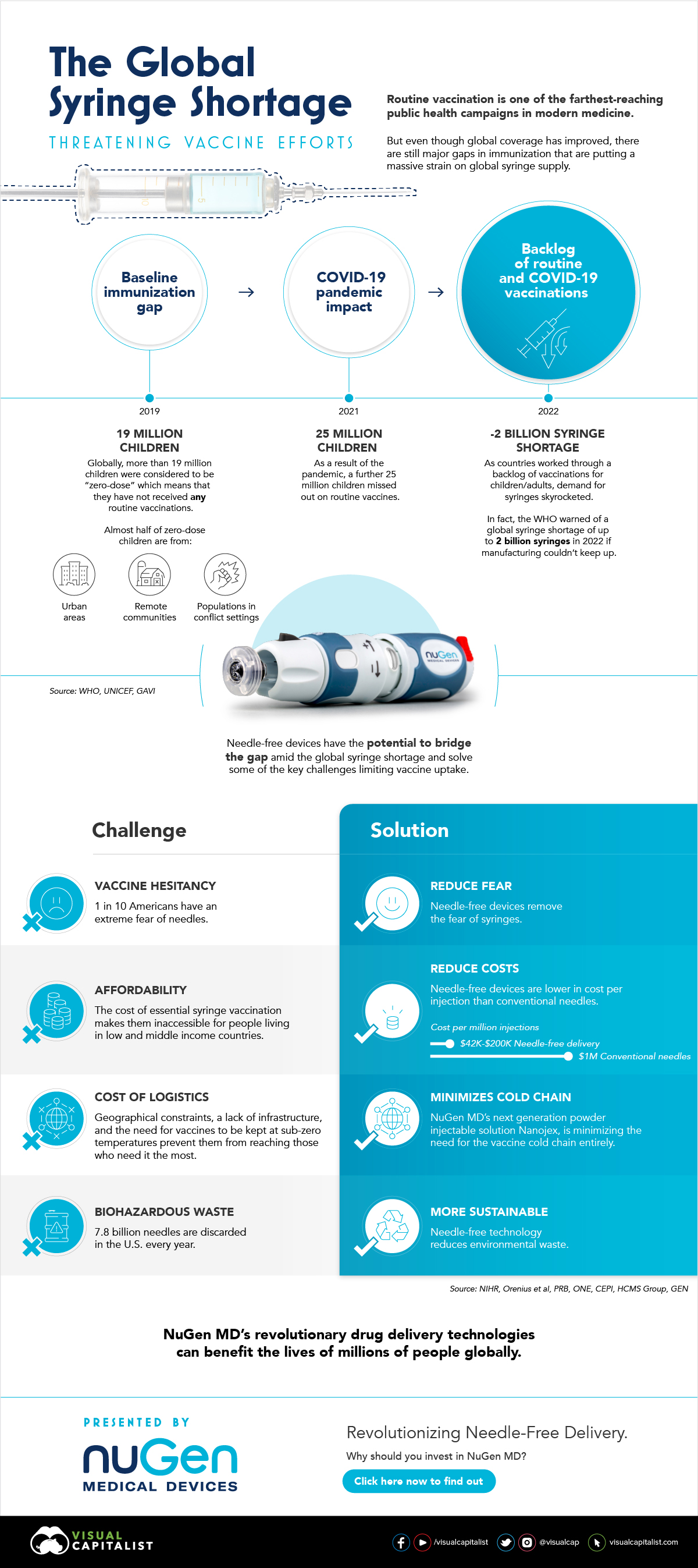
The Immunization Gap
Even before the COVID-19 pandemic, millions of people around the world struggled to get access to routine vaccinations. In fact, as of 2019 more than 19 million children around the world were considered to be “zero-dose” which means that they did not receive any routine vaccinations. Moreover, when the COVID-19 pandemic hit, global immunization dropped even further with 25 million children missing out on routine vaccines in 2021 alone.
Why is Immunization So Important?
Vaccinations prevent against over 20 life-threatening diseases and save between 2-3 million deaths per year, making them—as the WHO describes—the foundation of healthcare systems and an indisputable human right. As countries work through a backlog of vaccinations to close the immunization gap that has worsened since the pandemic, demand for syringes has significantly increased.
The Result: A Global Syringe Deficit
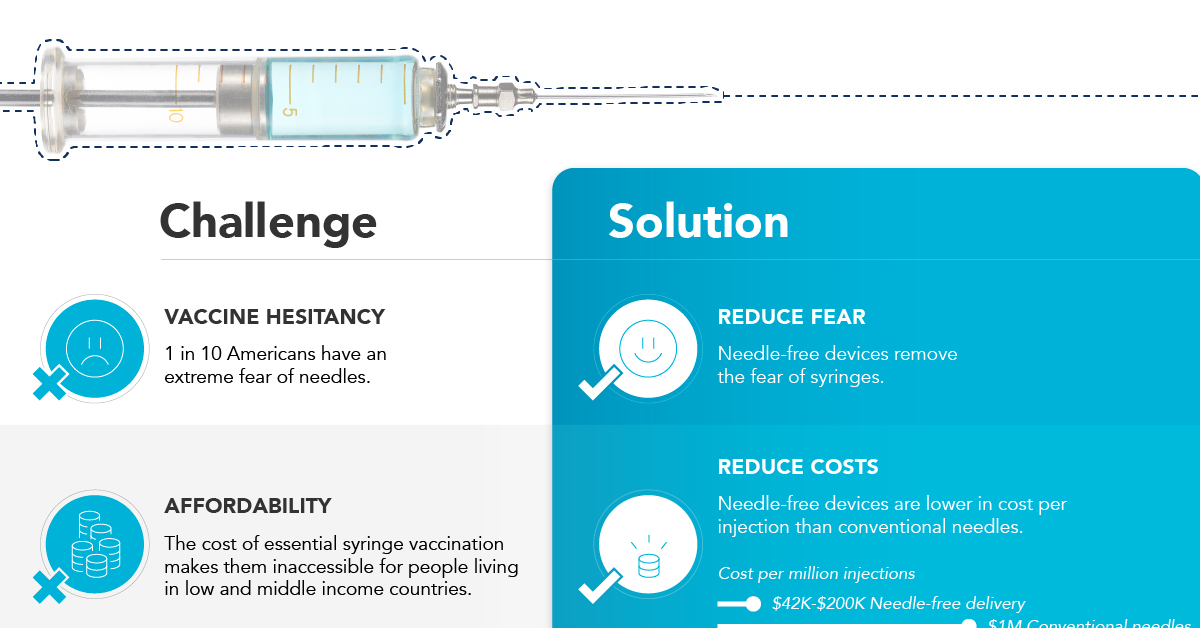
In 2022, the WHO warned that we could see a shortage of up to 2 billion syringes if manufacturing can’t keep up. This could result in the severe disruption to routine vaccinations and promote unsafe recycling of syringes in order to administer vaccines. But the issue goes far beyond a supply shortage of syringes. COVID-19 has brought conventional syringe vaccines into sharp focus, with many criticizing the challenges associated with them. With conventional needles facing so many challenges, it’s no surprise that investors are taking interest in viable alternatives. What’s more, these alternatives don’t just apply to vaccinations, they can also work for people with diabetes, dentists, and pet care.
Enter Needle-free Devices from NuGen MD
Needle-free devices have the potential to bridge the gap in immunization amid the global syringe shortage, solve some of the key challenges limiting vaccine uptake, and more importantly, benefit the lives of millions of people.
How Do They Work?
NuGen’s needle-free devices use a simple spring-loaded mechanism which uses pressure to release the liquid drug and penetrate the skin. In less than one-tenth of a second, the drug is dispensed more safely and evenly compared to needle syringes. It’s also virtually painless and leaves no mark on the skin.
Interested in investing in NuGen Medical Devices? To learn more about their plans to pioneer the future of needle-free drug delivery, click this link now.